New data of efficacy of a Meningococcal B Vaccine and a Preventive Antibiotic in Reducing the Risk of Bacterial STIs and proven efficacy of the MVA-BN Vaccine Against Mpox
Last updated on 28 February 2023
This study, sponsored and funded by ANRS | Emerging Infectious Diseases in partnership with Roche (1), was conducted by a research team from the Paris Public Hospitals Group AP-HP, Université Paris Cité, Inserm, and Sorbonne Université in collaboration with the associations AIDES and Coalition PLUS. It demonstrates the efficacy of both a meningococcal B vaccine in reducing the risk of gonorrhea infection and the use of the antibiotic doxycycline as a preventive treatment against sexually transmitted infections, when taken within 72h after sex. Following the first mpox cases in France, the study scope was expanded, adding the possibility to observe the efficacy of the Modified Vaccinia Ankara (MVA-BN) vaccine against the mpox virus responsible for the epidemic that emerged in 2022.
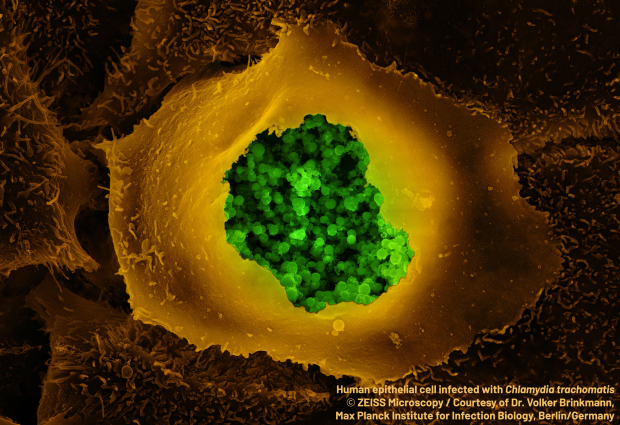
In recent years, France has seen an increase in sexually transmitted infections (STIs), including bacterial infections such as syphilis, chlamydia and gonorrhea, which particularly affect men who have sex with men (MSM). It was this population which has been mainly affected by the mpox epidemic, which emerged in France in May 2022.
The ANRS DOXYVAC trial was designed to evaluate interventions aimed at preventing these infections. It has been ongoing since January 2021 in MSM using PrEP to prevent HIV infection and highly exposed to the risk of STIs and having presented at least one STI during the year prior to their participation in it (2).
The ANRS DOXYVAC trial aims to measure the efficacy of an antibiotic and a vaccine in preventing bacterial STIs in MSM
Enrollment was stopped early and the two interventions were proposed to all participants following the promising results with doxycycline in the U.S. study DOXYPEP and at the recommendation of the data and safety monitoring board following an interim analysis requested by them.
The study is evaluating the efficacy of post-exposure prophylaxis (PEP) (3) for bacterial STIs that combines the antibiotic doxycycline and vaccination with Bexsero® against meningococcus B (4). Between January 2021 and July 2022, 502 MSM volunteers living in the Paris region were randomly assigned to into four groups: the first receiving doxycycline PEP to be taken within 72h after condomless sex; the second receiving vaccination with Bexsero®; the third a combination of these two interventions; and the fourth none of the two interventions.
The volunteers had a median age of 39 years, a median of 10 sexual partners in the last 3 months and received a median follow-up of 9 months. They were monitored and tested every 3 months for symptoms of gonorrhea, chlamydia and syphilis infections.
The researchers compared the incidence of a first episode of chlamydia or syphilis infection between the group that received doxycycline and the group that did not and found it to be 5.6 and 35.4 per 100 person-years (5), respectively (84% reduction in the risk of chlamydia or syphilis infection). As for the incidence of a first episode of gonorrhea infection in these same groups, this was found to be 20.5 and 41.3 per 100 person-years (51% reduction). After 3 months, the incidence of a first episode of gonorrhea infection in the Bexsero®-vaccinated group and the unvaccinated group was 9.8 and 19.7 per 100 person-years (51% reduction). No severe adverse effects relating to these two procedures were observed.
“The use of doxycycline for post-exposure prophylaxis has shown itself to be effective in reducing the incidence of both chlamydia and syphilis infection. This antibiotic has also had a significant impact, just like the meningococcal B vaccine, on the incidence of gonorrhea infections. This is the first time that a vaccine has shown an effect on a sexually transmitted bacterial infection,” concludes Prof. Jean-Michel Molina (Université Paris Cité and Department of Infectious Diseases at Hôpital Saint-Louis and Lariboisière, AP-HP, and Université Paris Cité), the study’s coordinating investigator.
Follow-up of the participants will continue until the end of 2023 to ensure that these prevention strategies, which have now been offered to all the participants, are effective in the medium term.
This study, which forms part of a global prevention effort, combines several risk reduction measures (repeated screening for HIV and STIs, vaccination against hepatitis A and B, distribution of condoms and gels). The participants also have the possibility to benefit from community support, therapeutic education, or both.
Beyond bacterial STIs, DOXYVAC has made it possible to analyze the impact of the MVA-BN vaccine on the incidence of the mpox virus rapidly after the appearance of the first cases
In France, the first cases of infection with the mpox virus appeared in May 2022. For the first time, the risk of human-to-human transmission of this virus through sexual contact has been observed. It has therefore been recommended since July 11, 2022 that the vaccine be used as a protective measure for multi-partner MSM.
In view of this observation, the research teams considered it necessary to include in DOXYVAC a component dedicated to studying the vaccine impact on the incidence of mpox virus in MSM taking PrEP, given that these volunteers are at risk of developing mpox. Among the 502 participants in DOXYVAC, the researchers analyzed, in this specific component, the information regarding 472 people whose data were available before and after May 8, 2022. These participants had reported having a median of 10 partners in the previous 3 months, and 20% had received a smallpox vaccine in childhood.
The researchers compared the pre-epidemic (i.e. until May 8, 2022) characteristics of the 77 volunteers having contracted mpox to the “control” volunteers who had not had the virus. They found that the cases of mpox affected younger people (37 vs. 40 years) who had had more sexual partners in the previous 3 months (7 vs. 5), and among whom fewer had been vaccinated against smallpox in childhood (4% vs. 23%). In people who did not have mpox infection, the proportion having had more than 10 partners over a 3-month period had decreased between the pre-epidemic and epidemic periods (up to and after May 8, 2022).
The incidence of mpox virus infection was 67.4 per 1 000 person-months between May 9 and July 10. It fell to 24.4 per 1 000 person-months between July 11 (date from which it was possible to get vaccinated) and September 20. The research team found that simply being vaccinated against the mpox virus in 2022 was associated with a reduced risk of developing the disease with an efficacy of 99%; the impact of behavioral change was limited in this highly vaccinated population (87%). “This vaccine provides a high level of protection against the mpox virus,” explains Prof. Jade Ghosn (Université Paris Cité, Department of Infectious and Tropical Diseases of Bichat-Claude-Bernard Hospital AP-HP), DOXYVAC co-investigator and the researcher behind the implementation of the study’s “mpox” component.
AIDES, which has developed numerous risk reduction tools during the mpox crisis and participated in providing community support in these studies, welcomes these results. For Camille Spire, president of the association, “the emergence of new effective tools to add to the existing prevention arsenal is to be welcomed, especially since during the mpox crisis we have noted a high level of vaccine uptake by the people exposed to the virus. We will work to ensure that the effective accessibility of these tools is supported by public policies in terms of the fight against STIs“.
Vincent Leclercq, managing director of Coalition PLUS adds: “in order to achieve their full potential, these prevention tools must reach all the populations at which they are targeted. However, access to vaccines and medicines is too often restricted to the richest countries. We have seen it with the mpox epidemic: only the countries of the North have been able to set up vaccination campaigns“.
1. Roche Molecular System and Roche Diagnostics France provided – free of charge – the kits, consumables and reagents needed to detect Chlamydia trachomatis, Neisseria gonorrhoeae and Mycoplasma genitalium.
2. These men are participants in the HIV infection prevention cohort ANRS PREVENIR.
3. Post-exposure prophylaxis (PEP) is the use of preventive treatment in people who have recently been exposed to a risk of disease transmission to prevent them from developing it.
4. Meningococcus B (Neisseria meningitidis) is a bacterium that can cause meningitis. It is close to gonococcus (Neisseria gonorrhoeae).
5. X per 100 person-years: this means that out of 100 patients followed up for one year, there is a probability of observing X events (in this case an STI).
Find out more
- ANRS 174 DOXYVAC: an open-label randomized trial to prevent STI in MSM on PrEP
Jean-Michel Molina (1), Béatrice Bercot (2), Lambert Assoumou (3), Michèle Algarte-Genin (3), Emma Rubenstein (1), Gilles Pialoux (4), Christine Katlama (5), Laure Surgers (6), Cécile Bébéar (7), Nicolas Dupin (8), Jean-Paul Viard (9), Juliette Pavis (10), Claudine Duvivier (11), Jade Ghosn (12), Dominique Costagliola (3)
- Impact of vaccination on mpox incidence in MSM on PrEP in the ANRS 174 DOXYVAC trial
Jade Ghosn (12), Lambert Assoumou (3), Moussa Ouattara (3), Michèle Algarte-Genin (3), Emma Rubenstein (1), Gilles Pialoux (4), Christine Katlama (5), Laure Surgers (6), Claudine Duvivier (11), Juliette Pavis (10), Jean-Paul Viard (9), Séverine Gibowski (13), Manon Ollivier (13), Dominique Costagliola (3), Jean-Michel Molina (1)
1. Université Paris Cité, Saint-Louis Hospital (AP-HP), Department of Infectious and Tropical Diseases, Paris
2. Université Paris Cité, Infection, Antimicrobials, Modeling and Evolution (IAME), Functional Unit of Bacteriology, National Reference Center for Bacterial STIs, Saint-Louis Hospital (AP-HP), Paris
3. Sorbonne Université, Inserm, Pierre Louis Institute of Epidemiology and Public Health, Paris
4. Sorbonne Université, Hôpital Tenon (AP-HP), Department of Infectious and Tropical Diseases, Paris
5. Sorbonne Université, Pitié-Salpêtrière Hospital (AP-HP), Department of Infectious and Tropical Diseases, Paris
6. Sorbonne Université, Inserm JRU S1136, Pierre Louis Institute of Epidemiology and Public Health, Saint-Antoine Hospital (AP-HP), Department of Infectious and Tropical Diseases, Paris
7. Université de Bordeaux, Department of Bacteriology, National Reference Center for Bacterial STIs, Bordeaux University Hospital, Bordeaux
8. Université Paris Cité, Cochin-Port-Royal Hospital (AP-HP), Department of Dermatology, Paris
9. Université Paris Cité, Hôtel-Dieu Hospital (AP-HP), Department of Immunology and Infectious Diseases, Paris
10. Université Paris Cité, Hôtel-Dieu Hospital (AP-HP), Department of Clinical Immunology, Paris
11. Université Paris Cité, Necker-Enfants-malades Hospital (AP-HP), Department of Infectious and Tropical Diseases, Paris
12. Université Paris Cité, Bichat-Claude-Bernard Hospital (AP-HP), Department of Infectious and Tropical Diseases, Paris
13. ANRS | Emerging Infectious Diseases, Paris
Press contacts
ANRS | Maladies infectieuses émergentes: information@anrs.fr
AP-HP: service.presse@aphp.fr
Université Paris Cité: presse@u-paris.fr
Sorbonne Université: claire.de_thoisy-mechin@sorbonne-universite.fr
Inserm: presse@inserm.fr
AIDES: mcherrid@aides.org
Coalition PLUS: drojascastro@coalitionplus.org
