COVID-19
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus.
Last updated on 14 March 2025
In brief
- Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus.
- Infection with this virus, which can sometimes cause severe respiratory disease, can have health repercussions in the medium to long term.
- Since the emergence of the virus, many variants and successive epidemic waves have been observed.
Origin of COVID-19
History
At the end of the year 2019, there had been reports of several cases of atypical pneumonia in the city of Wuhan, China. The emergence of a new coronavirus – initially named nCoV-2019 – was suspected.1
Sequencing has shown that this coronavirus shares 80% of its genome with that of SARS-CoV, responsible for previous human epidemics.1,2 However, with 88% identity, its genome turns out to be closer to those of the bat-SL-CoVZXC21 and bat-SL-CoVZC45 coronaviruses isolated in 2015 and 2017 from bats.2 The zoonotic* origin of the new coronavirus renamed SARS-CoV-2 was then strongly suspected, with the bat being the animal reservoir and the pangolin likely to be the intermediate host.1,2
In early 2020, the emerging infectious disease called COVID-19 (short for coronavirus disease 2019) and caused by SARS-CoV-2, took on pandemic proportions. As of 8 July 2020, over 11.8 million infections had been recorded with at least 544 000 deaths worldwide.2
This pandemic has been responsible for an unprecedented global health and economic crisis.1
According to Johns Hopkins University, SARS-CoV-2 had caused over 670 million cases of COVID-19 and 6.8 million deaths from the time of its appearance up to March 2023.3 The mortality rate is currently estimated at between 1 and 2%. However, it is certainly lower, given that many asymptomatic cases are not included in the total number of infected individuals.4 The high number of deaths observed is therefore a consequence of the large size of the human population.4
The COVID-19 virus
SARS-CoV-2, short for severe acute respiratory syndrome coronavirus, is a coronavirus that causes COVID-19, a respiratory infection.
- The coronaviruses
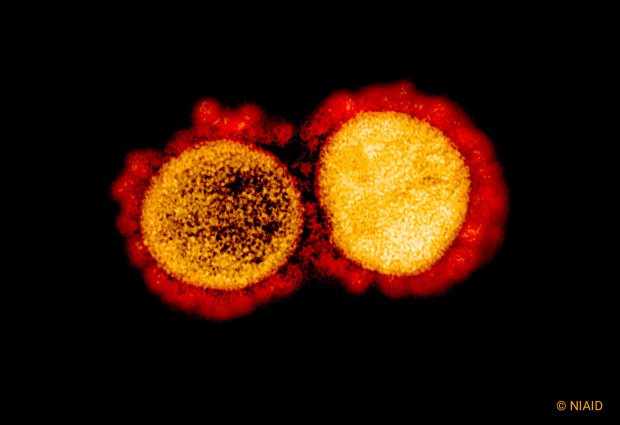
Coronaviruses are enveloped, roughly spherical structures that measure between 80 and 200 nm in diameter, with positive-sense single-stranded RNA**.1,5 The spike (S) proteins form a large crown (corona) on their surface and the N proteins, closely linked to the genomic RNA, form the nucleocapsid. The M and E proteins make up the membrane and envelope.5
The coronaviruses belong to the Coronaviridae family, a group of RNA viruses known to infect four of the seven classes of vertebrates: mammals, birds, amphibians and bony fishes.6 There are seven that are currently capable of infecting humans (HCoV).5 Four are responsible for upper and lower respiratory infections, which are generally mild; the other two, SARS-CoV and MERS-CoV (Middle East respiratory syndrome-related coronavirus), highly pathogenic, have emerged recently.5
The Coronaviridae family comprises two subfamilies: Coronavirinae and Torovirinae. Coronavirinae are divided into four genera: Alpha-, Beta-, Gamma- and Deltacoronavirus. Human coronaviruses (HCoV) belong to the Alpha– and Betacoronaviruses. The Betacoronavirus genus is subdivided into four clades: A, B, C and D.5
- SARS-CoV-2 and its variants
SARS-CoV-2 belongs to clade B, like SARS-CoV, which appeared in 2003.5 However, phylogenetic analyses have shown it to be closer to the coronaviruses that affect bats (bat-SL-CoVZXC21 and bat-SL-CoVZC45).2,5
The SARS-CoV-2 genome consists of around 30 000 bases, making it the longest known RNA virus genome.1,2
SARS-CoV-2, like all pandemic viruses, has the ability to evolve in the host through a ‘quasispecies’ process, which is specific to RNA viruses: due to their low replication fidelity, RNA viruses produce, in the same host and for each generation, a large population of different mutant viruses (variants).4
SARS-CoV-2 is therefore highly genetically diverse. However, while virtually all variants are unviable and therefore eliminated,4 the virus can acquire a certain number of genes that code for proteins enabling it to enrich its adaptive potential.5 The gene encoding the surface S protein, which binds to the cell receptor and is the epitope of the neutralising antibodies, is the one that undergoes the strongest selection.5 Significant changes in the form of the spike and therefore its function, depending on whether they modify neutralisation sites and/or cell attachment sites, facilitate or on the contrary reduce the transmissibility of the virus and/or the immune response to viral infection.7
The pandemic context, with mass epidemic outbreaks in areas of high population density, has undoubtedly created favourable conditions for the emergence of SARS-CoV-2 variants.8
The WHO has classified them into two groups: Variants of Interest (Eta, Iota, Kappa, Lambda whose spread is limited) and Variants of Concern (Alpha, Beta, Gamma, Delta) responsible for serious infections and a high risk of mortality.7
The historic strain of SARS-CoV-2 from Wuhan has virtually disappeared. It has been successively replaced by different variants. In France, the Delta variant from India, more contagious and having become predominant in the world, was replaced at the end of 2021 by the Omicron variant (sublineage BA.1), which emerged in southern Africa. In comparison to Delta, Omicron has higher transmissibility and, most importantly, a greater immune escape. Since late February 2022, Omicron’s BA.2 sub-lineage has in turn become predominant.9
* from an animal host with transmission to humans; ** a positive RNA can be translated directly into proteins

Transmission
A pandemic virus
SARS-CoV-2 is a pandemic virus: it is multi-host, capable of infecting individuals of different species.4 It recognises the ubiquitous Angiotensin Converting Enzyme 2 (ACE2) cell receptor involved in blood pressure regulation and cardiac and renal homeostasis in vertebrates.4
To be pandemic, a virus must have ‘relatively low pathogenicity’ with a significant incubation period, thereby promoting its transmission in the population.4 This is the case with SARS-CoV-2.4
Modes of transmission
COVID-19 has four modes of transmission. Three are direct – from person to person:10
- By droplets and/or
- By aerosols* emitted by an infected person
- By direct contact (through hands)
The fourth mode is indirect, and is by contact with a contaminated inert surface. Transmission takes place when unwashed hands are brought into contact with the eyes, nose or mouth.10,11
According to currently available data, the vast majority of transmissions occur by direct contact at short distances (usually within one metre), via droplets.10,11 Airborne transmission by aerosols, which remain suspended in the air or move over distances greater than one metre (long distance)11, can take place under special so-called ‘opportunistic’ circumstances (e.g. during medical procedures on the respiratory sphere of infected patients).10 It can also occur when the circumstances are lend themselves to this: such as shouting or singing for a prolonged period of time in a confined, unventilated or poorly ventilated room with many people who are not taking protective measures.10
COVID-19 distinguishes itself from other respiratory infections with its potential transmission by asymptomatic or pre-symptomatic individuals.9 They are responsible for 50-80% of infections.10
In addition, with COVID-19, the number of secondary transmissions generated from an index case** is highly heterogeneous. The majority of index cases do not lead to any transmission. Only a small minority leads to many cluster transmissions, known as ‘superspreader events’.10
The genetic diversity of the virus also plays a role in transmission. As a result, the Alpha and Delta variants of SARS-CoV-2 presented a higher transmission potential than the original strain.10
* suspension in the air of liquid and/or solid particles, which are smaller than droplets; ** the first person to be diagnosed with the new disease. Identification of the index case is often retrospective. The primary case is the first person to be infected by a given virus. Between the onset of the primary case and that of the official index case, the virus spreads undetected (due to a lack of established diagnosis) in the human population.10
Symptoms and treatment
Symptoms
The main symptoms, whether combined or isolated, are the same as those of acute respiratory infections:12
- Fever or feeling of fever, chills, sweating
- Respiratory signs: cough, shortness of breath, sore throat, tightness in the chest, having a cold
- Headache, muscle aches, unusual tiredness
- Diarrhoea
Sudden loss of smell (without nasal obstruction) and/or total loss of taste are also suggestive signs of COVID-19. For elderly people, there is a sudden change in general condition, the appearance or worsening of mental capacity, a state of confusion, repeated falls, a rapid worsening of an already known disease.12
In the vast majority of cases, COVID-19 is low-risk, often without signs. But it can be very serious, especially in people aged 65 and over, people who are obese or rendered vulnerable by certain chronic diseases, and pregnant women.13 However, the disease may worsen after a few days, with increasing respiratory discomfort that requires oxygen. Other complications may occur, affecting the liver, heart and brain.13
The signs may last for weeks or even months. This is referred to as long COVID. It even occurs in people who have had mild forms. Specialised follow-up with rehabilitation may be necessary.13
The mortality observed during the pandemic is most often not directly linked to a pathogenic effect of the virus, but rather to the frailty of patients who died and who were generally elderly and/or with major comorbidities.4 Worldwide, 80% of those who died were aged 60 years and over.13

Diagnosis
Diagnosis can be direct by reverse transcription polymerase reaction (RT-PCR) or indirect by blood sampling.14 For detection of the SARS-CoV-2 genome by RT-PCR or of some of its proteins by antigen tests and self-tests, several types of sampling may be performed:14
- Nasopharyngeal sampling using a swab inserted deep into the back of the nose
- Nasal sampling with a swab inserted into the nose
- Oropharyngeal sampling from the back of the throat
- Saliva test performed in the mouth
Nasopharyngeal sampling is the technique that enables better detection of the virus by RT-PCR.14
The majority of individuals infected with SARS-CoV-2 develop an adaptive humoral immune response*. Serological tests performed after blood sampling detect the production of immunoglobulins directed against the virus.5 If COVID-19 is suspected, it is also possible to get tested in a pharmacy or in a medical biology laboratory, or to perform a self-test available from a pharmacy.12
Treatments
- Antivirals
Nirmatrelvir/ritonavir (Paxlovid) is indicated in adult patients who do not require oxygen therapy and who are at high risk of progressing to a severe form of COVID-19.12,15 This treatment is particularly indicated, regardless of vaccine status, in patients of any age with immunosuppression or severe disease, or in people aged 65 and over, with risk factors for developing severe forms.12 Remdesivir is prescribed in second-line if Paxlovid is formally contraindicated and in the absence of contraindications, including renal contraindications.16
- Monoclonal antibodies
For severe forms, oxygen, corticosteroids and sometimes antibodies may be used.13 Monoclonal antibodies are injectable drugs that specifically target the spike protein of SARS-CoV-2.16 They are associated with risks of infusion-related reactions and hypersensitivity reactions. In addition, there have been increased reports of cardiovascular and/or thromboembolic events with them.16
Monoclonal antibodies must only be used on the basis of official recommendations taking into account the epidemiological context and activity data on circulating SARS-CoV-2 variants.16
- Pain medicines
For patients at low risk of hospitalisation, pain medicines such as paracetamol can be used to relieve fever or pain, combined with rest and drinking plenty of fluids.13,17
* specific immune response mainly related to B-cell function
Prevention
In people at risk of a severe form of COVID-19, prevention is based on the maintenance of all precautionary measures:12,15,18
- Washing hands with soap and water or rubbing them with hand gel to prevent the spread of germs
- Airing of rooms to prevent transmission of the disease through the air
- Wearing a mask to prevent the spread of germs around you
For all eligible individuals, prevention is based on the administration of vaccine booster doses according to the latest recommendations.15
As soon as symptoms suggestive of COVID-19 appear, it is strongly recommended, in addition to protective measures, to apply the following individual preventive measures:12
- Encourage telework where possible
- Inform and avoid close contact with vulnerable people
Whenever possible, in the event of incapacitating symptoms affecting daily or professional activities, it is advisable to stay at home during the contagious period (on average 5 to 7 days depending on the viral infection).12
Vaccines
Vaccination, which immunises individuals against a pathogen responsible for the disease, is necessary to stem the COVID-19 pandemic. Once the SARS-CoV-2 genome sequence was known, vaccine development progressed very rapidly, with a first clinical trial conducted in March 2020.19
Messenger RNA vaccines
The messenger RNA (mRNA)* technique has been studied and tested for several years.19 It consists of injecting not the whole virus but its mRNA.20
The mRNA in COVID-19 vaccines is produced by the in vitro transcription of a synthetic DNA sequence, or cloned into plasmid DNA, encoding the S protein of the virus. As mRNA is highly unstable, its structure is stabilised by various modifications. It is then encapsulated in lipid nanoparticles (LNP) that will be injected.19
Following injection of the vaccine containing the encapsulated mRNA, the antigen-presenting cells (APCs) having ingested the particles translate the mRNA thanks to their cell machinery. The viral antigenic protein produced will trigger a specific immune response. mRNA vaccines are particularly effective in activating B cells located in the germinal centres of lymph nodes and inducing their differentiation into virus-specific memory B cells and into plasma cells producing antibodies with a long lifespan.19,21
The messenger RNA is then rapidly eliminated. It never enters the cell nucleus and never changes our DNA.20
Vaccines available in France
COVID-19 mRNA vaccines are highly effective, even if no vaccine offers 100% protection. Their efficacy, which is variable, depends on the individual and the variant. Vaccines protect primarily against severe forms of the disease and protect less well against the disease itself, or against transmission of the virus when infected.13 Transmission in vaccinated individuals, even if it decreases, is therefore still possible. As such, it is necessary to continue to use precautionary measures.13
The vaccines currently available in France are for the Omicron variant, which appeared at the end of November 2021 and circulates virtually exclusively in the country. There are three vaccines:13
- Comirnaty Omicron JN1, RNA vaccine, indicated in people 12 years of age and older
- Comirnaty Omicron JN1 (paediatric), RNA vaccine, indicated in children from 5 to 11 years of age
- Comirnaty Omicron JN1 (paediatric), RNA vaccine, indicated in children from 6 months to 4 years of age
* mRNA is the intermediate genetic material in the gene expression process. In our cells, mRNA is produced by transcription from our DNA and translated into proteins
Research: The actions of ANRS EMI
During the crisis, ANRS MIE (Emerging Infectious Diseases) facilitated, evaluated, coordinated and funded French research into COVID-19. The emergence of variants of SARS-CoV-2, whose characteristics are likely to modify the dynamics of the epidemic and the response to treatments or vaccines, has highlighted the essential role of genome surveillance.
To address these challenges, the agency is coordinating two major projects: EMERGEN at national level and AFROSCREEN in 13 African countries.
EMERGEN and EMERGEN 2.0
EMERGEN is a flagship project set up in 2021 in response to the health crisis related to the emergence of COVID-19. Coordinated by ANRS MIE and Santé publique France on French territory, both mainland and overseas, EMERGEN has significantly strengthened sequencing capacities in France. It was when this consortium was set up that the Flash Surveys were activated with the aim of mapping the SARS-CoV-2 variants circulating in France at a given time.
EMERGEN 2.0 was created in 2023 as part of the national EID acceleration strategy. It aims to perpetuate this infrastructure between crises and open it up to other emerging or re-emerging infectious pathogens.
AFROSCREEN
The AFROSCREEN project was launched in 2021 as a response programme to the COVID-19 epidemic and was subsequently extended to include other emerging pathogens.
It has been designed as a network to:
- improve epidemic preparedness and response at national and regional levels
- support decision-makers in defining public health priorities
- produce data to fuel the international public health effort
The project, funded by the French Development Agency (AFD), is coordinated by a consortium of three French institutions (ANRS EID, Institut Pasteur and IRD) and has 25 national public health partner institutions located in 13 African countries.
The COVID-19 clinical research platforms
With the COVID-19 crisis, Inserm and ANRS EID have actively mobilised to support the establishment of clinical trial platforms and facilitate the initiation of studies in France, Europe and Africa.
- I-REIVAC-Emergen – platform for the clinical trial of vaccines for emerging pathogens including SARS-CoV-2
- DisCoVery – a European platform for therapeutic trials in the context of EU-RESPONSE for COVID-19
- ANTICOV – a platform to identify treatments for moderate forms of COVID-19 in Africa and South America
Consult the COVID-19 Emergence Unit
References
- Juckel D, et al. Les coronavirus, ennemis incertains. Médecine/sciences 2020 ; 36 : 633-641. https://www.medecinesciences.org/en/articles/medsci/full_html/2020/06/msc200147/msc200147.html. (consulté le 23/01/2025)
- Sallard E, et al. Retrouver les origines du SARS-CoV-2 dans les phylogénies de coronavirus. Médecine/sciences 2020 ; 36 : 783-796. https://www.medecinesciences.org/en/articles/medsci/full_html/2020/07/msc200195/msc200195.html. (consulté le 23/01/2025)
- COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. COVID-19 Map – Johns Hopkins Coronavirus Resource Center. (consulté le 23/01/2025)
- Frutos R, et al. Le virus SARS-CoV-2 n’a pas « d’origine ». Médecine/sciences 2022 ; 38 : 600-607. https://www.medecinesciences.org/en/articles/medsci/full_html/2022/06/msc220021/msc220021.html
- Lefeuvre C, et al. Aspects virologiques et diagnostic du coronavirus Sars-CoV-2. Actualités pharmaceutiques 2020 ; 599 : 18-23. https://www.sciencedirect.com/science/article/pii/S0515370020302962. (consulté le 23/01/2025)
- Woo PCY, et al. Family: Coronaviridae. J Gen Virol 2023;104(4). https://www.microbiologyresearch.org/content/journal/jgv/10.1099/jgv.0.001843. (consulté le 23/01/2025)
- Rouzioux C. Les variants du SARS-CoV-2 face au dépistage et aux vaccins. Bull Acad Natl Med 2022 ; 206 : 215-218. https://www.em-consulte.com/article/1498446/les-variants-du-sars-cov-2%C2%A0face-au-depistage-et-au. (consulté le 23/01/2025)
- Lina B. Les différentes phases de l’évolution moléculaire et antigénique des virusSARS-CoV-2 au cours des 20 mois suivant son émergence. Bull Acad Natl Med 2022 ; 206 : 87-99. https://www.em-consulte.com/it/article/1493691/les-differentes-phases-de-l-evolution-moleculaire-. (consulté le 23/01/2025)
- Covid-19. https://www.inrs.fr/publications/bdd/eficatt/fiche.html?refINRS=EFICATT_Covid-19. (consulté le 23/01/2025)
- Birgand G, et al. Modes de transmission du SARS-CoV-2 : que sait-on actuellement ? Médecine et Maladies infectieuses Formation 2022 ;1 : 2-12. https://www.sciencedirect.com/science/article/pii/S2772743221000015. (consulté le 23/01/2025)
- Organisation Mondiale de la Santé. Maladie à coronavirus 2019 (COVID-19) : comment se transmet la COVID-19 ? https://www.who.int/fr/news-room/questions-and-answers/item/coronavirus-disease-covid-19-how-is-it-transmitted. (consulté le 23/01/2025)
- Ministère du travail, de la santé, des solidarités et des familles. Tout savoir sur le covid-19. Tout savoir sur le Covid-19 – Ministère du Travail, de la Santé, des Solidarités et des Familles. (consulté le 23/01/2025)
- Vaccination InfoService.fr. Covid-19. https://vaccination-info-service.fr/Les-maladies-et-leurs-vaccins/Covid-19. (consulté le 23/01/2025)
- Haute autorité de la santé. Covid-19 : quel test faire ? Haute Autorité de Santé – Covid-19 – Quel test faire ? (consulté le 23/01/2025)
- Fiche : Réponse rapide dans le cadre de la covid-19. Traitement de la covid-19. HAS et ANRS MIE, 21 juin 2023. https://www.has-sante.fr/upload/docs/application/pdf/2023-06/reco468_fiche_rr_traitement_covid_19_mel.pdf. (consulté le 23/01/2025)
- Point sur l’utilisation des traitements contre le covid-19. https://ansm.sante.fr/actualites/point-sur-lutilisation-des-traitements-contre-le-covid-19-disponibles-en-acces-precoce? (consulté le 23/01/2025)
- Organisation Mondiale de la Santé. L’OMS met à jour ses lignes directrices sur les traitements contre la covid-19. https://www.who.int/fr/news/item/10-11-2023-who-updates-guidelines-on-treatments-for-covid-19. (consulté le 23/01/2025)
- Ministère du travail, de la santé, des solidarités et des familles. Les gestes barrières, des réflexes simples pour se protéger et protéger ses proches face aux virus de l’hiver. https://sante.gouv.fr/prevention-en-sante/preserver-sa-sante/pour-un-hiver-sans-virus/article/les-gestes-barrieres-des-reflexes-simples-pour-se-proteger-et-proteger-ses. (consulté le 23/01/2025)
- Feraoun Y, et al. Covid-19, des vaccins à la vitesse de l’éclair. Médecine/sciences 2021 ; 37 : 759-772. https://hal.science/hal-03321924. (consulté le 23/01/2025)
- Vaccination InfoService.fr. Les évolutions en cours et l’avenir de la vaccination. https://vaccination-info-service.fr/Generalites-sur-les-vaccinations/Histoire-de-la-vaccination/Les-evolutions-en-cours-et-l-avenir-de-la-vaccination. (consulté le 23/01/2025)
- Couvreur P. Délivrance de l’ARN à l’aide de nanoparticules lipidiques. Bull Acad Natl Med 2022 ; 206 : 1208-1218. Délivrance de l’ARN à l’aide de nanoparticules lipidiques – ScienceDirect. (consulté le 23/01/2025)
Publications
- Planchais C, et al. Potent human broadly SARS-CoV-2-neutralizing IgA and IgG antibodies effective against Omicron BA.1 and BA.2. J Exp Med 2022
- Fenwick C, et al. Patient-derived monoclonal antibody neutralizes SARS-CoV-2 Omicron variants and confers full protection in monkeys. Nat Microbiol 2022
- Marlin, RD, et al. Antiviral Efficacy of Favipiravir against Zika and Sars-Cov-2 Viruses in Non-Human Primates. Nat Commun 2022
- Colosi E., et al. Screening and vaccination against COVID-19 to minimise school closure: a modelling study. Lancet Infect Dis 2022
- Ndongo FA, et al. Rapid Increase of Community SARS-CoV-2 Seroprevalence during Second Wave of COVID-19, Yaoundé, Cameroon. Emherg Infect Dis 2022.
- Grant R, et al. Impact of SARS-CoV-2 Delta variant on incubation, transmission settings and vaccine effectiveness: Results from a nationwide case-control study in France. Lancet Reg Health Eur 2022


